
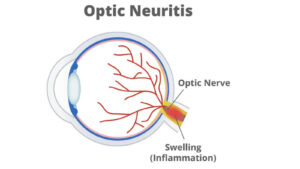
The diagnosis of MS [1] typically relies on the presence of neurological signs and symptoms, alongside evidence from magnetic resonance imaging (MRI) scans of lesions within the central nervous system (CNS). In 2001, an international team of neurologists developed a set of guidelines [2] to integrate MRI data with clinical and laboratory evaluations to establish a diagnosis of MS. These ‘gold standard’ McDonald diagnostic criteria have been subsequently updated in 2010 and 2017 following scientific advances in the field of MS, and further updates may occur in the future as our knowledge continues to expand. Indeed, during the 38th Congress of ECTRIMS [3] in October 2022, emerging evidence in support of the inclusion of optic nerve lesions in the McDonald criteria was discussed. Given that optic neuritis is a fundamental feature of MS, and the first clinical demyelinating event in approximately a quarter of individuals with MS, its inclusion in the McDonald criteria may be the next logical step forward. In this issue of ECTRIMS Insights, we will consider how the diagnosis of MS has progressed and the challenges that physicians continue to face, particularly in the differential diagnoses of different subtypes of MS.
Reaching consensus in the diagnosis of MS
 The publication of the revised McDonald criteria in 2017 [4] provided an updated consensus framework with which to establish a definitive diagnosis of MS. According to these criteria, a diagnosis of MS can be confirmed if individuals have evidence of CNS damage that is disseminating in space and in time. Although the latest amendments to the criteria did not change the diagnosis of MS, they were intended to permit a diagnosis to be made earlier in the disease course, thereby providing the individual with earlier access to appropriate treatment. The extensive reliance on MRI data within the criteria have driven a recommendation that an MRI scan is performed for any individual for whom a diagnosis of MS is possible, particularly given that CNS lesions may be observed in the absence of clinical symptoms.
The publication of the revised McDonald criteria in 2017 [4] provided an updated consensus framework with which to establish a definitive diagnosis of MS. According to these criteria, a diagnosis of MS can be confirmed if individuals have evidence of CNS damage that is disseminating in space and in time. Although the latest amendments to the criteria did not change the diagnosis of MS, they were intended to permit a diagnosis to be made earlier in the disease course, thereby providing the individual with earlier access to appropriate treatment. The extensive reliance on MRI data within the criteria have driven a recommendation that an MRI scan is performed for any individual for whom a diagnosis of MS is possible, particularly given that CNS lesions may be observed in the absence of clinical symptoms.
As a consequence of the updates made to the McDonald criteria, the guidelines published by the Middle East North Africa Committee for Treatment And Research in Multiple Sclerosis (MENACTRIMS) [5] were also revised, with the focus being on the exclusion of all other possible entities that could underlie the patients’ signs and symptoms. Such a consistent application of diagnostic recommendations around the globe could be an important step towards equity of treatment for all individuals with MS.
Challenges in the diagnosis of MS remain
 Diagnosis of MS can be challenging given that there is no single test that will provide a definitive diagnosis. Rather, as noted above, a diagnosis of MS is often only made once other conditions have been excluded. Earlier diagnosis has reduced the incidence of patients with clinically isolated syndromes [6] and it has been suggested that radiological isolated syndromes, that is the occurrence of lesions consistent with demyelination in the absence of symptoms, should also be considered as part of the disease course of MS. Careful assessment of all available clinical, paraclinical and radiological data [7] can assist in the exclusion of other conditions, thus reducing the diagnostic challenges that have previously existed and helping to remove some of the barriers to early disease-modifying treatment for individuals with MS.
Diagnosis of MS can be challenging given that there is no single test that will provide a definitive diagnosis. Rather, as noted above, a diagnosis of MS is often only made once other conditions have been excluded. Earlier diagnosis has reduced the incidence of patients with clinically isolated syndromes [6] and it has been suggested that radiological isolated syndromes, that is the occurrence of lesions consistent with demyelination in the absence of symptoms, should also be considered as part of the disease course of MS. Careful assessment of all available clinical, paraclinical and radiological data [7] can assist in the exclusion of other conditions, thus reducing the diagnostic challenges that have previously existed and helping to remove some of the barriers to early disease-modifying treatment for individuals with MS.
However, challenges remain, not least the differential diagnosis [8] of the different subtypes of MS. In time, it is possible that such challenges will be overcome, perhaps due to the development of novel biomarkers as discussed in the December issue of ECTRIMS Insights [9]. In addition, the integration of additional factors, such as optic nerve lesions, into diagnostic systems like the McDonald criteria may, in time, facilitate the improved identification of MS. Other challenges can include the misunderstanding and misapplication of the McDonald criteria [10]. Therefore, there may be an ongoing need to not only develop diagnostic tools to refine the diagnosis of MS, but also to ensure a comprehensive communication of these tools together with adequate training in their use by relevant healthcare professionals.
Promoting continued advances in research
ECTRIMS welcomes this continued research to improve the accuracy of diagnosis, and facilitate early diagnosis, for individuals with MS. We applaud the efforts of the scientific community to constantly improve our understanding of early signs and symptoms of MS. Such advances may ultimately improve diagnosis, permitting earlier treatment and so halting disease progression and optimising patient care. We remain optimistic that ongoing research will continue to improve our knowledge of how best to treat individuals with all types of MS and provide a personalised approach to care.
***
ECTRIMS Insights articles are produced with an intent of being a neutral source of information sharing and objective analysis for the MS and neuroscience community. Unless otherwise stated, cited information in our articles does equivocate official endorsement from ECTRIMS.
***
REFERENCES
[1] Brownlee WJ, et al. Lancet. 2017;389(10076):1336–1346.
[2] Multiple Sclerosis News Today. Guidelines for MS Diagnosis: McDonald Criteria. Available at: https://multiplesclerosisnewstoday.com/ms-diagnosis-mcdonald-criteria/. Accessed March 2023.
[3] ECTRIMS 2022. 38th Congress of the European Committee for Treatment and Research in Multiple Sclerosis. Available at: https://2022.ectrims-congress.eu/. Accessed March 2023.
[4] Thompson AJ, et al. Lancet Neurology. 2018;17(2):162–173.
[5] Yamout B, et al. Mult Scler Relat Disord. 2020;37:101459. doi: 10.1016/j.msard.2019.101459.
[6] Sørensen, P. Current Opinion in Neurology. 2021;34(3):275–276.
[7] Calabrese M, et al. Current Opinion in Neurology. 2021;34(3):277–285.
[8] Kling J, et al. Neurology Reviews. 2023. Available at: https://www.mdedge.com/neurology/article/261497/multiple-sclerosis/differential-diagnosis-ms-what-watch. Accessed March 2023.
[9] ECTRIMS Insights. Can biomarkers help us move towards a more holistic approach to tackling MS? 2022. Available at: https://www.ectrims.eu/insights/can-biomarkers-help-us-move-towards-a-more-holistic-approach-to-tackling-ms/. Accessed March 2023.
[10] Solomon AJ, et al. Mult Scler. 2021;27(2):250–258.